BBetter Home Page › Forums › Ask Your Questions › Lab Tests, Markers & Interpretations › GI map results
-
GI map results
Posted by ami_dancing on February 20, 2024 at 2:49 amHello! I would love your feedback on my GI map results. Thank you so much for taking the time to look them over and help me understand them!
/
ami_dancing replied 8 months, 1 week ago 2 Members · 8 Replies -
8 Replies
-
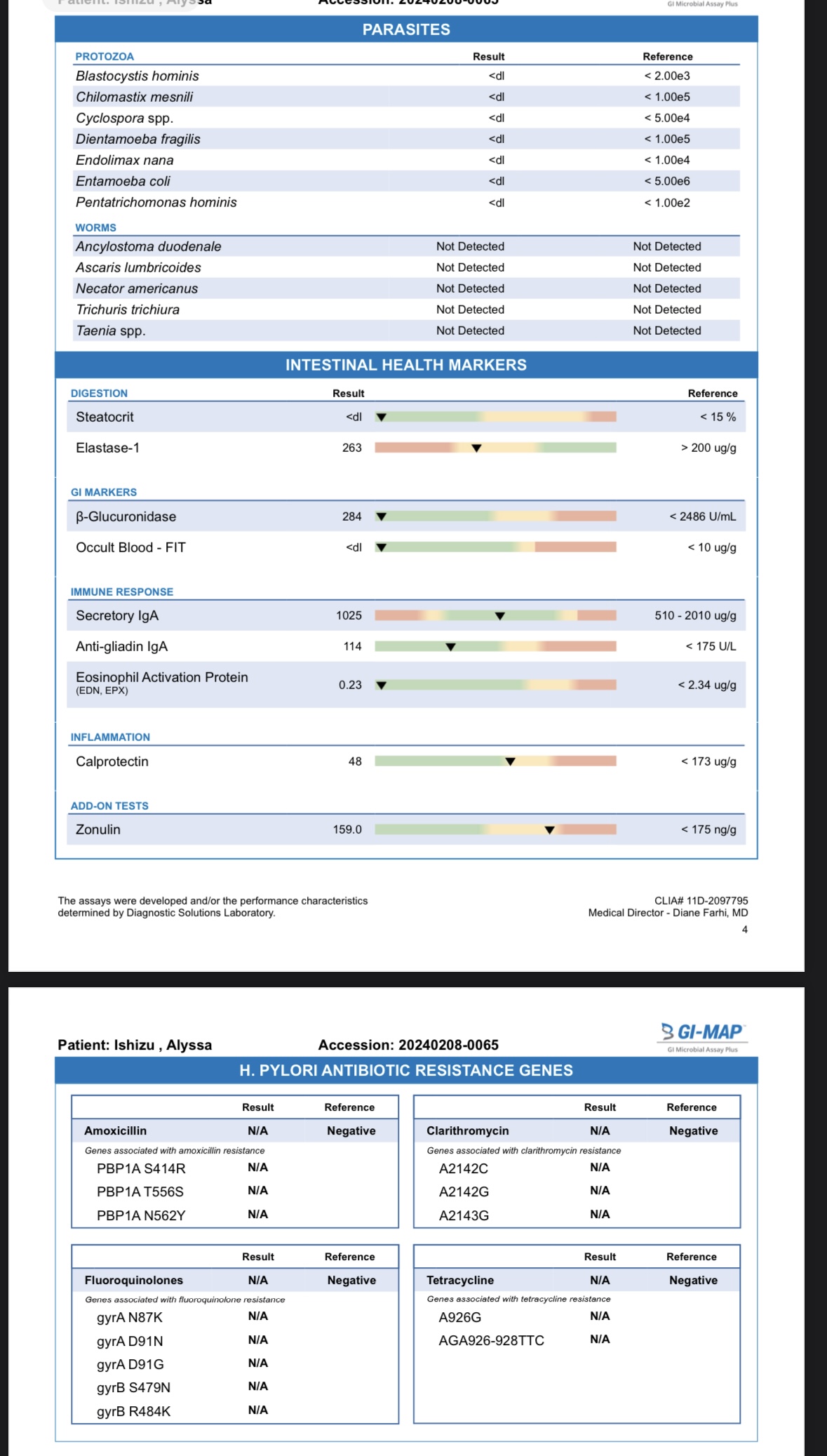
Hi @Alyssa Ishizu ok let’s start with the intestinal health markers on p.4 and then I’ll jump around.
Elastase 1 helps us determine if there’s maldigestion and / or hypochlorhydria (low stomach acid). Ideally, I like to see this above 500, so in your case, this could point to insufficient stomach acid triggering the release of digestive enzymes, or a need to support pancreatic function. How is your diet and do you know your blood sugar status by any chance (fasting glucose, fasting insulin, HbA1C)?
Although your H Pylori marker is considered negative, it may still be high enough to create symptoms of hypochlorhydria. Please watch THIS VIDEO in the Gut Health Masterclass course and let me know so I can guide you further. I would also encourage you to watch THIS VIDEO to uncover other root cause reasons for low stomach acid.
Back to p.4, anti-gliadin. Gliadin is a component of gluten, the protein found in wheat and other field grass grains such as barley, malt, and rye. The presence of fecal antigliadin antibodies can indicate an immune response (in the gut) to gluten in the diet. Your levels aren’t clinically high, but it’s creeping up there. The suggested solutions when there’s an elevation in anti-gliadin sIgA is to consider eliminating gluten 100% for at least 4 months while healing the gut lining. If you are already gluten-free, consider sources of gluten and gliadin cross-reactive food such as dairy, corn, oats, millet, rice and yeast. Here’s the handout on gluten elimination, and here’s a video on gut healing therapies.
Calprotectin – calprotectin is the most studied marker of gastrointestinal inflammation. While yours isn’t clinically high, it is inching it’s way up and we’d like it to be as close to zero as possible. Higher calprotectin could indicate neutrophil (immune cell) infiltration to the gut mucosa. So basically the immune system is reacting to something such as intestinal infections, proinflammatory dysbiosis (imbalance in the microbiome), food allergies, toxins and certain drugs (e.g., non-steroidal anti-inflammatory drugs [NSAIDs]), etc. So obviously, the goal is to remove anything that’s causing an immune response; removing food sensitivities and addressing the possible causes. Also consider anti-inflammatory support (e.g., anti-inflammatory diet, curcumin, omega-3 fatty acids, aloe, and resveratrol). If you’d like to pursue additional testing, the KBMO food sensitivity test can provide insight into which foods may be causing an inflammatory response, and help remove trial and error.
Zonulin is a protein that opens intercellular tight junctions in the gut lining (the connections between epithelial cells that make up the gastrointestinal lining). Zonulin increases intestinal permeability in the jejunum and ileum and is considered a biomarker for barrier permeability (aka leaky gut). Your is not clinically high, but you can see it’s borderline high. Again, the removal of gluten would help since gluten increases zonulin. Removing food sensitivities as well, all while supporting with gut healing herbs as mentioned above. Ensuring vitamin D levels are optimal would be helpful as well. Have you measured it recently?
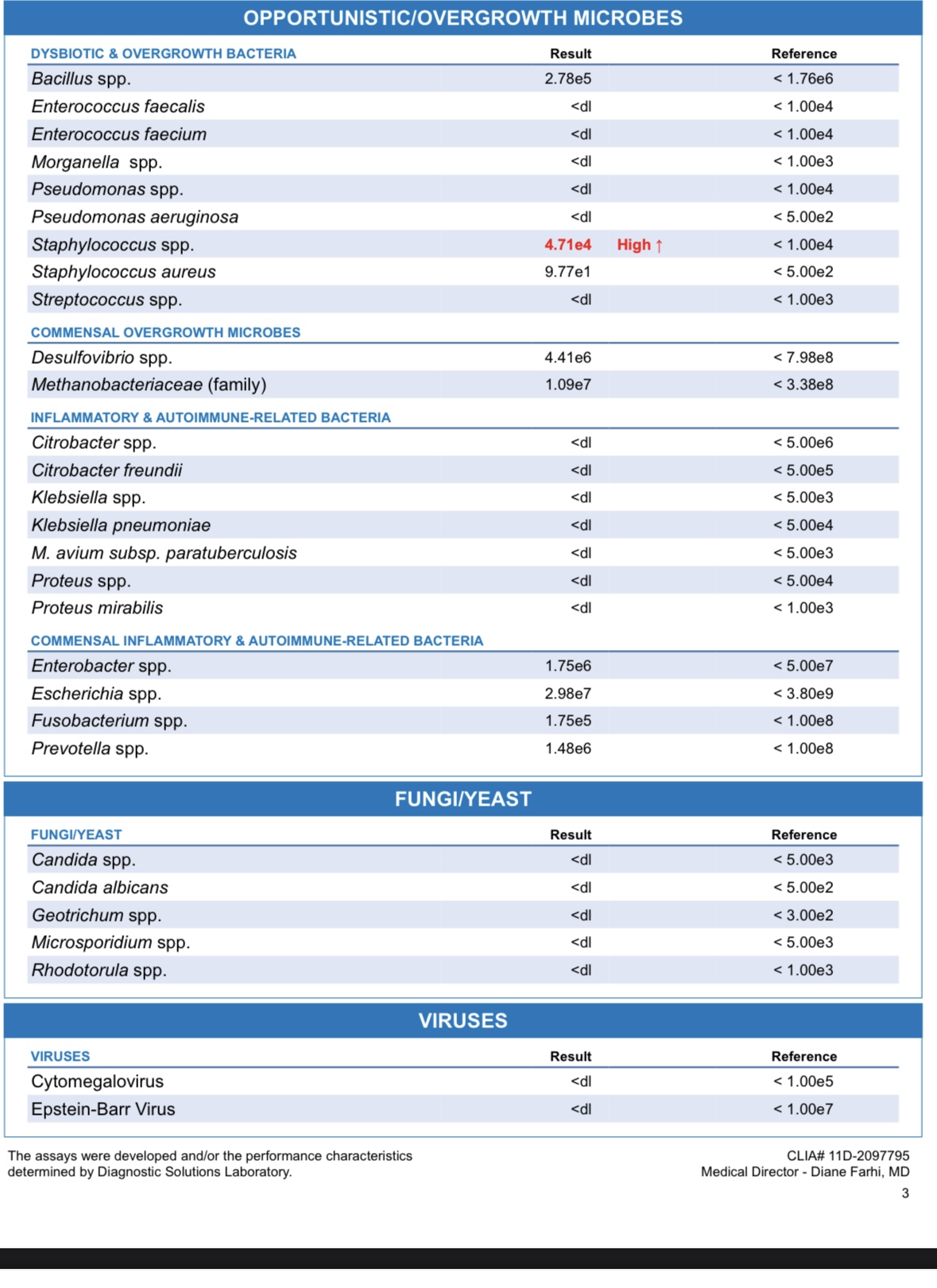
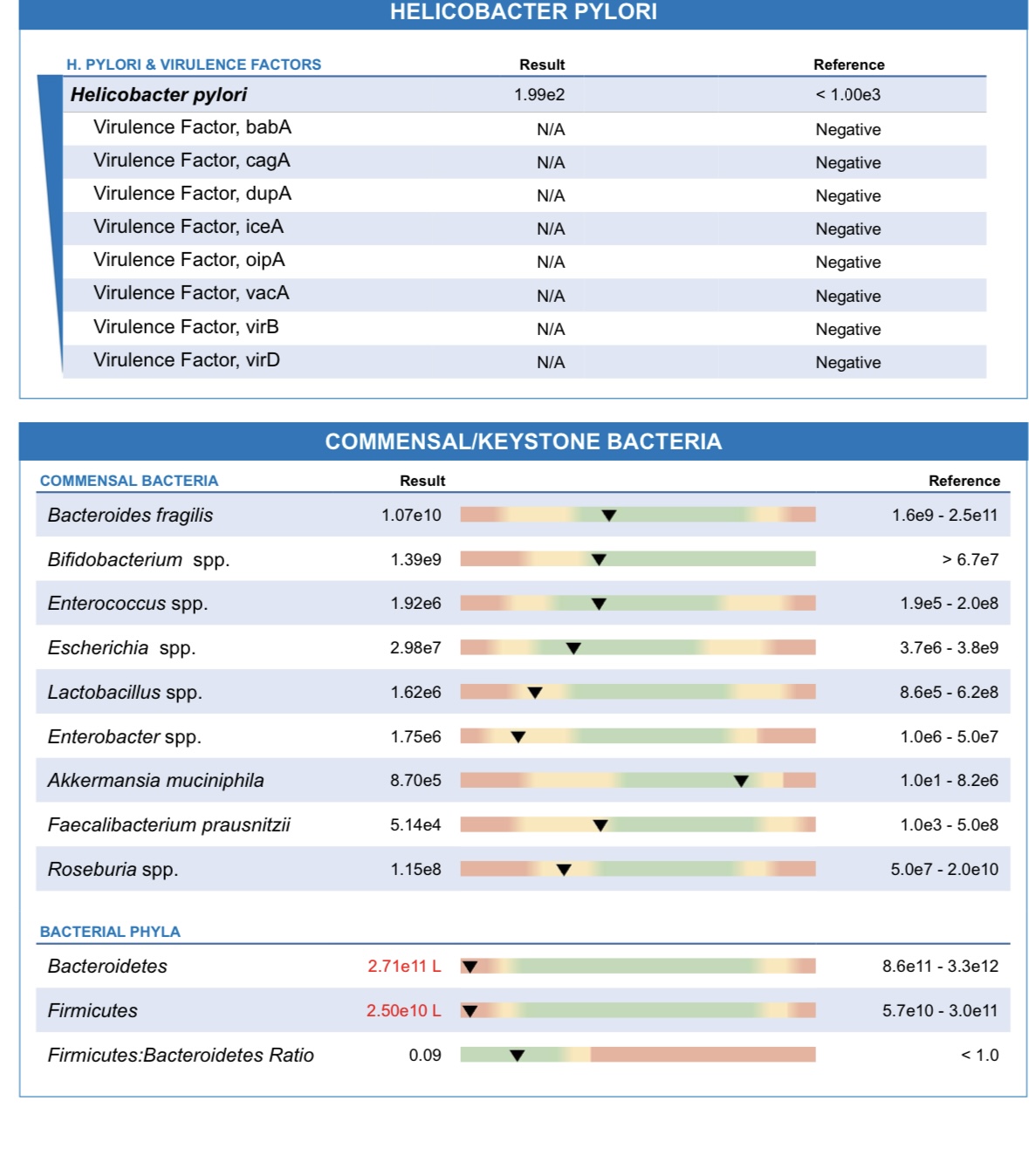
Now looking at your commensal bacteria, you can see that both firmicutes and bacteroidetes are both clinically low. This means your “good bacteria” are low. This could happen for a number of reasons such as frequent antibiotic use, certain medications, low fiber diet, and so on.
Eating a variety of fermented foods if tolerated (kimchi, sauerkraut, beet kvaas, kefir) daily can help bring in more beneficial bacteria. We have recipes for all of these HERE. A broad spectrum, diverse probiotic formula, 50-450 billion CFUs/day can also help bring on board better diversity.
Increasing dietary intake of vegetables and fibers (psyllium, oat bran)
Remove dietary sugar and refined carbohydrates
Prebiotic supplementation (resistant starch, xylooligosaccharide, inulin, beta-glucan, arabinogalactan)
Reduce inflammation as discussed above
Please answer my questions above, and I can help guide you further.
-
Hi! Thank you so much for the feedback!! So helpful!
I’ll try to keep things in order as I answer your questions.
Elastase 1-
I do not know my blood sugar status.
I did the baking soda test for stomach acid and it was a terrible, nothing at all as far as burping within the 5 min window! yikes. I do have bloating a lot, although I don’t usually have stomach pain. Gas can be on and off, I am not always sure why / if it’s a particular food that causes a period of time that I have a lot of gas and then some periods of time when I don’t but that seems to be a cycle.
I tend to eat a lot of rice, chicken, veggies and eggs.
I am not sure about the H.Pylori. Since the number is on the higher side would that point to HPylori or do you think it is more indicating the low stomach acid? What do you suggest for helping with stomach acid and the H.Pylori?
Anti – Gliadin
I eat 80% gluten free, but will do as you suggested and go for 100%. I eat rice and corn and occasionally dairy. (no oats, millet or minimal yeast) Do you suggest I cut these as well?
Zonulin
Vit D – I have not had that tested recently, however I do live in a very cloudy city and in the winter getting sun exposure is a challenge! I have a supplement that I take that is to help with that.(might need more!)
Commensal Bacteria
Very interesting! I am adding in fermented foods. Is there a prebiotic supplement that you recommend?
I was wondering about the Staphylococcus spp. and Staphylococcus aureus, as their numbers were also high. Would that be in part because of the low amount of good bacteria and if that is supported then the others would be brought down?
I have been going through your Gut health masterclass, which is also helpful, trying to understand the best way to support and heal my gut!
Thank you so much for your help!
-
@Alyssa Ishizu well done for going through the Gut Health Masterclass course – it will definitely help you understand your gut better so you can start to support the main digestive players.
In clients who are symptomatic (bloating, stomach pain, gas) and fail the baking soda test, I will usually recommend addressing the H Pylori when it’s nearing clinical high. An H Pylori overgrowth is a common root cause reason for low stomach acid, and low stomach acid will compromise digestion further down south, including the release of pancreatic enzymes and bile.
So you can find H Pylori protocols HERE (make sure you watch the video taken from the Gut Health Masterclass and read the different protocols beneath the video). Generally, I find that doing a course or two of Matula tea protocol to be very gentle and effective.
After at least 3 weeks on an H Pylori protocol, it’s then a good idea to consider supporting stomach acid with HCL Betaine to prevent a recurrence of H Pylori overgrowth. THIS handout shares instructions on how to do the dosing challenge to find the right dose for a individual’s unique needs.
Now keep in mind that HCL betaine support is temporary and for rapid relief. What’s important is to figure out what created or is creating the low stomach acid environment in the first place. Based on THIS video (Causes of Hypochlorhydria), what do you think is at play in your case? Please let me know.
To answer your question about eliminating grains and dairy, the best way to know is to do an elimination challenge of each and taking notes of how you feel when these foods are eliminated fully for at least 30 days. Here’s a handout on how to perform an elimination challenge and reintroduction. If that seems daunting and you have the financial means for testing, you can consider the KBMO food sensitivity test to see which specific foods are causing an inflammatory response.
If you’re going to supplement with vitamin D, it’s always best to test your levels before so you know how much to take and for how long. Here’s a helpful handout to help with dosing vitamin D.
Regarding the commensal vs opportunistic species. Some bacterial and fungal species will take advantage of situations and if given the opportunity to overgrow and take over the playing field (i.e. the gut microbiome), they will.
In your case, both Staphylococcus spp. and Staphylococcus aureus are gram-positive bacteria in the Firmicutes phylum. High levels may result from reduced digestive capacity, and intestinal inflammatory activity. Since there’s likely hypochlorhydria and reduced digestive enzyme output, this could be the environment that’s allowing these opportunistic species to take over. So again, figuring out what’s causing hypochlorhydria in the first place is the root cause approach.
The good news is that when you increase the commensal bacteria through eating more fermented foods and/or broad spectrum probiotics, the immune system is better at modulating the microbiome and keeping overgrowths from happening. Ensuring vitamin D, A, and zinc are optimal can help immunity as well. These can all be measured in blood. Best to get RBC zinc and not serum zinc if possible.
In terms of probiotic supplements, I share a few of my favorites in THIS VIDEO from the Gut Health Masterclass course. Starting off with fermented foods (if tolerated) and transient probiotics is usually how I start my clients off, and if doing good, then add in soil based after 60-90 days for another 60-90 days.
Hope this helps. Will wait to hear your reply on what you believe may be the cause of hypochlorhydria in your case.
-
Hi!
I have watched your video on the cause of Hypochlorhydia several times, but still don’t have clarity on what the exact cause of H.Pylori would be for me! My best guesses are sympathetic dominance and possibly deficiency in zinc and B vitamins, excess sugar / carbs. I am not on any medications and don’t drink alcohol. I have not been on any antibiotics for as long as I can remember, (possibly in my childhood / under 18, but I don’t recall) I have taken a fair amount of Ibuprofen through my teen and early twenties as a way to manage period cramps, before I understood more about alternative ways to address those issues. Could that be part of the issue?
Thank you for the additional resources for eliminating foods and reintroducing etc.
I found bloodwork for Vit D from Sep of 2023 and my number was 62. I realize that was a while back now, but at least a small reference point. The handout was helpful!
I am ordering the Gastromend- HP and LactoBif Probiotics 100Bllion CFU. The Matula tea sounds amazing but I think I will try these other supplements and hope that they work!
As you suggested, after 3 weeks of Gastromend -HP then I will try to introduce the Betaine after that and hope that will help jumpstart my body to produce enough HCL on its own. I realize it is a tempoary solution and wondered how long you recommend I take it? (I realize I am a ways off from that point yet but through I’d check)
Very grateful for your insight and help!
-
@Alyssa Ishizu trust your gut instinct regarding the causes of hypochlorhydria. Are you still under a lot of stress? This is often a big factor that can keep people from truly getting well because we’re not designed to be in a sympathetic state all the time. Naturally, when the body is stressed, all digestive secretions are reduced, which can give H Pylori (an endemic bacteria) the opportunity to overgrow and further contribute to hypochlorhydria. So focusing on stress reduction measures is key. There are many ways to help the body “feel safe”. If you’d like to share more about the stressors in your life, I’d be happy to offer tools and therapies that might help.
Why do you suspect zinc and B vitamins are at play? Do you not consume enough animal proteins? Zinc is commonly measured in blood. If you can get an RBC zinc, that would give a better indication of cellular zinc (vs. what’s in the blood at the time of the blood draw) and the need to supplement or not. I also like to measure copper and ceruloplasmin along with zinc since copper and zinc compete with each other. This could help you figure out if zinc insufficiency is potentially a cause.
The same with B vitamins. It’s possible to test serum vitamin B12 but keep in mind that it’s affected by what you consume the night before testing. So avoid B supplements and zinc/B-rich foods at least two days before testing to get a better baseline measure. For serum B12, I like to see it above 600pg/mL.
Regarding excess sugar/carbs, I find that when my clients start adopting the VPF+C principle, their cravings for carbs and sugar disappear because the body is properly fueled with the macronutrients it needs and blood sugar levels are stable. You can learn more about my VPF+C principle HERE inside the Beginner’s Health Roadmap course. You can also watch the diet analysis video to help you apply the VPF+C principle to your diet, and then watch dealing with cravings to help you make necessary tweaks. Happy to take a look at your food journal (which is attached in the diet analysis video).
Regarding the dosage and duration of HCL supplementation, it really depends on whether or not you’ve addressed the cause. But what I can say is that most of my clients are on it for at least 3 months, and over time their body starts to tell them when to reduce the dosage because they’ll start to experience a mild burning sensation. That’s a good sign, and just means that it’s time to reduce the dosage. You can read THIS handout on how to do the HCL dosage challenge.
Let me know if you have any other questions, and if you’d like to share about the stressors.
-
Hello! I apologize for the delay in responding!
Stress – I feel that might be a huge part of my issues. I tend to internalize stress and realize that is a contributing factor. While I love my job (I am a professional ballet dancer & teacher), it does require a lot not just physically but also mentally. Sometimes a stressor. Also, the past 2 years I have been walking through traumatic grief with the passing of my mom from cancer.
Open to any tools you can suggest for managing and helping me give my body the ’safe’ feelings etc
Thank you for the tips and feedback on Zinc and B vitamins. I struggle with fatigue (could be more adrenal related) , hair loss on and off and combined with the digestion issues (constipation /diarrhea back and forth). Your testing suggestions are helpful to figure out the exact ranges. I don’t have any blood work with that already.
I have been working to incorporate more protein in my meals and your VPF+C principals / videos have been helpful! I think in general I don’t get enough protein and am trying to up that. I also think that I might need to be eating more frequently to make sure my blood sugar does not dip too low.
I have started taking LactoBif 100 1x a day, in the morning before I eat breakfast
As well as GastroMend-HP as directed on the bottle 4 per day, split and between meals( 2 /2) So far I don’t know that I feel any significant changes, except possibly more bloated? It has been less than 1 week of taking both. I just realized that I need to also have the broccoli sprouts supplement to go with it, so I have not started that one yet.
Appreciate your feedback about the HCL supplementation. I will stay on the GastroMend-HP for 1 month and hope that it addresses the H.Pyloi well and I can then move on from that.
Thank you again, I really appreciate your feedback and insight. Very helpful!
-
@Alyssa Ishizu
Very sorry to hear about your mom. EMDR therapy can be very effective at disassociating from traumatic experiences. Doing in-person Neo Emotional Release therapy, and body work can also be helpful at releasing trapped emotions. You can learn more about these healing modalities HERE from the Adrenal Balance course.
If there’s also hair loss, low energy and IBS, it’s also a good idea to test your thyroid function if you’re planning on getting labs done. And stress/adrenals impact the thyroid, so again, stress reduction should be your priority.
Regarding your diet – I’m glad the videos were helpful. If you’re needing to snack in between your main meals, ask yourself if you’re eating enough (portion wise), and also ask if you’re getting in enough proteins and healthy fats. If someone is insulin resistant, more frequent meals are helpful, but ideally, we should give our digestive system a rest in between our main meals, and therefore not be snacking. This allows the MMC (our migrating motor complex) time to do a “clean sweep” of the small intestine to prevent bacterial overgrowths. Constant snacking is often one of the biggest culprits of SIBO/IBS. So just keep that in mind, and ensure you’re getting at least 3-4 hours of digestive rest if you can between meals.
If you’re noticing more bloating since starting the probiotic, it might help to go slower. So perhaps taking it every other day for example to allow your microbiome the chance to adjust. Also, changing the time of day might be helpful. I normally recommend my clients to take their probiotics in the evenings or before bed.
Please keep us posted on how you’re doing, and let us know if you have any other questions.
-
Thank you so much!
I will go with your recommendation to switch the time of day I take the probiotic and see if that helps.
I appreciate your input and am really trying to look at my whole body to see how best to support it.
Thank you for sharing so much and I will keep you updated as I go!
Log in to reply.