-
Posted by yasminatassi on May 29, 2024 at 2:18 pm
Hello B
Am 42, and almost all my life I have struggled with some sort of acne issue . I tried everything ( even reccutane when I was in my early 30’s) the only time that my skin looked amazing was when I got pregnant 2 years ago and then continued until again now it comes back with acne again . It usually comes around the time am ovulating which makes me think it’s an androgen issue , I eat super clean no sugar lots of fruits and veggies , protein etc . I am getting quite fed up and need some Guidance pls . I searched the forum and found some tips here and there including the article that @Daniel which was helpful but I can’t access fullscript
Here are rfecent tests I done that might be helpful / am preatty fed up so any advice or things to take wouod be super appreciated as I thought I got rid of the problem once I got pregnant !
Bernadette replied 7 months ago 3 Members · 15 Replies -
15 Replies
-
Hi @Yasmin atassi , I recently started too look deeper into acne and possible root causes because of my daughter….
Have you ever checked your gut health? Is your liver struggling? What about personal care and make up?
Acne needs inner work as well as what we put on our skin.
I also learnt that not all clean products are necessarily non pore clogging, another cause for acne.
Just a few ideas where to start looking -
Hi @Yasmin atassi – thanks for sharing your test results.
I’m going to share some education and also ask you additional questions so that we can puzzle piece together. Deal?
First, please watch THIS VIDEO on the role of DHEA in our body from the Adrenal Balance course.
Next, please read THIS Symptom Dictionary handout on Acne to look at the most common root cause factors.
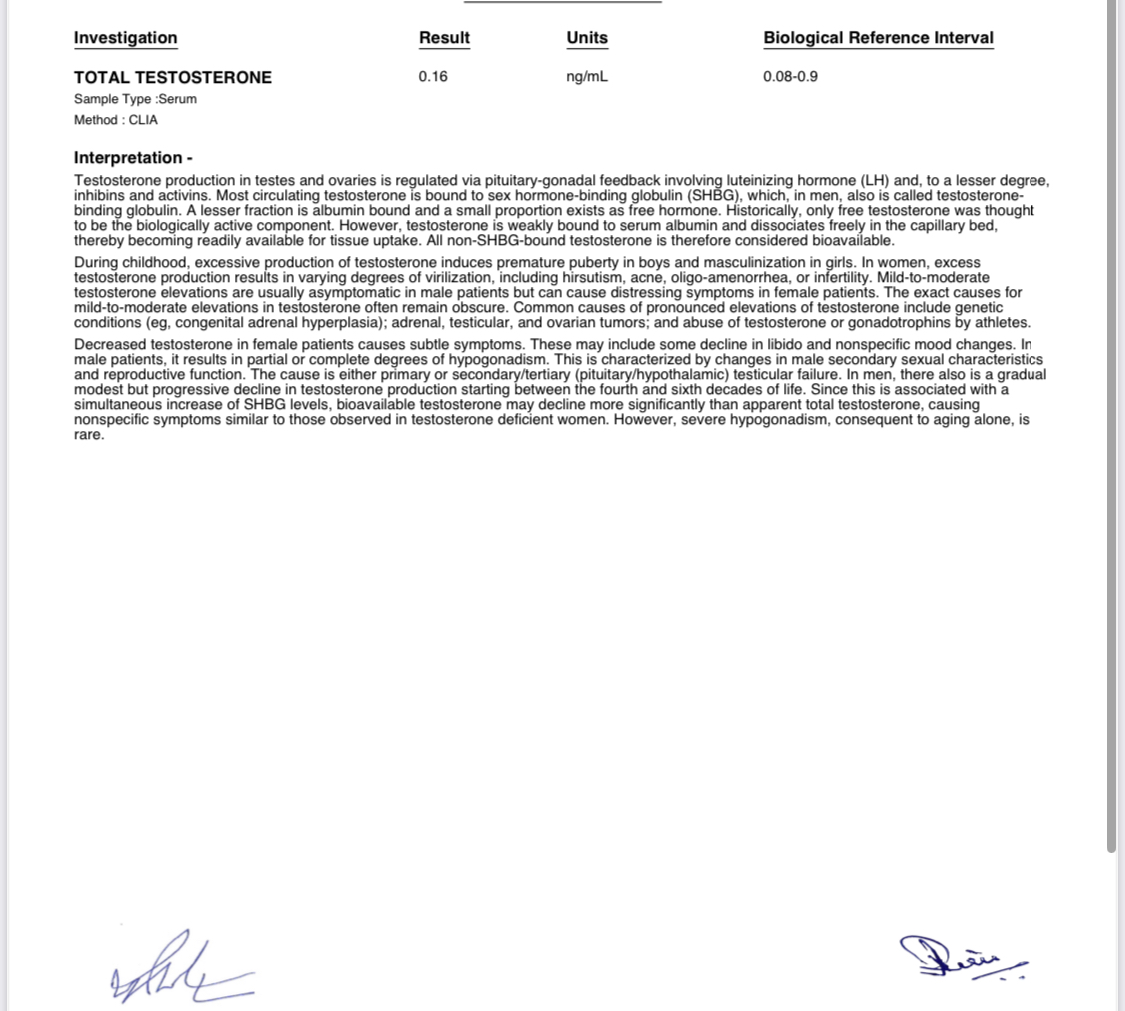
You provided a very valuable clue about the acne improving when you were pregnant, and then reappearing post-partum. During a successful pregnancy, progesterone increases the most in order to maintain the uterine lining and prevent miscarriage or premature labor. Estrogen levels, particularly estriol, also rises significantly, to support fetal development and maternal body changes.
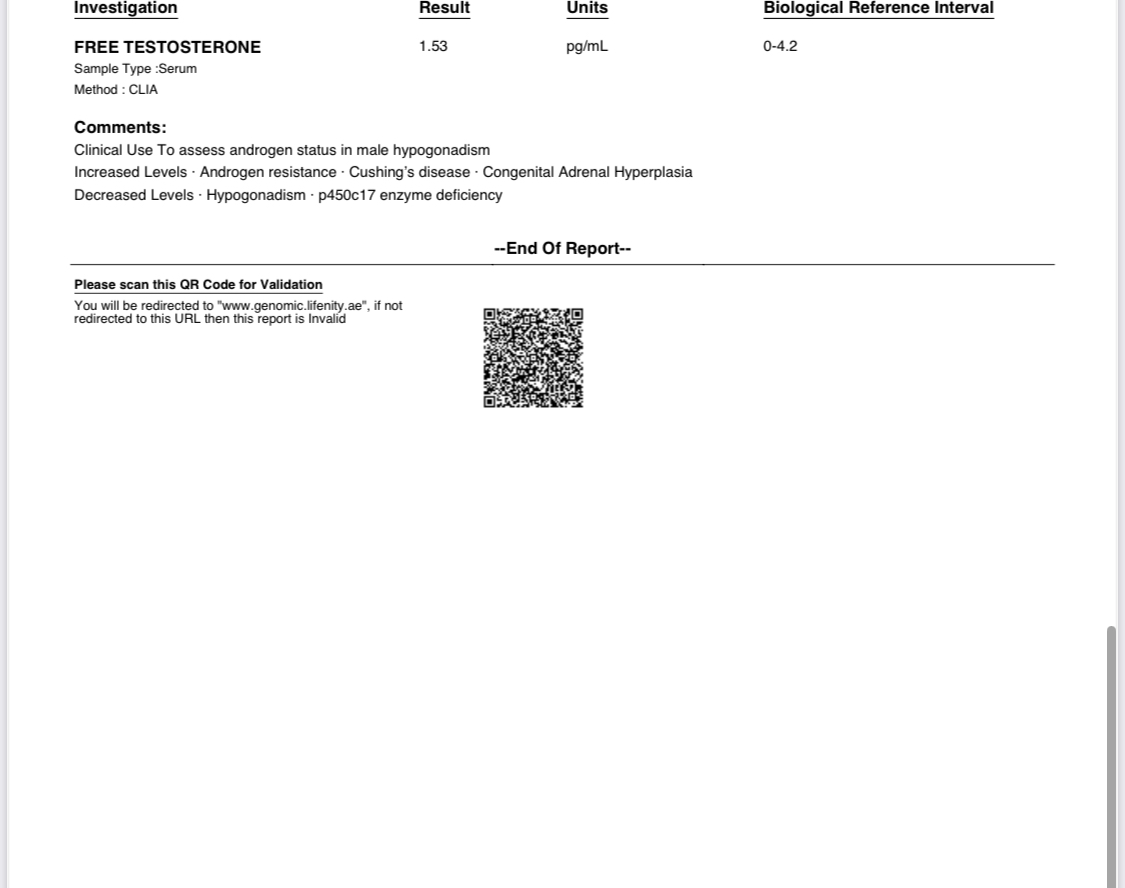
Therefore, if someone was androgen dominant before pregnancy, meaning testosterone is relatively higher than both estrogen and progesterone, then the natural increases of both estrogen and progesterone during pregnancy will improve that ratio/hormonal balance. This could explain why you felt relief during pregnancy. Makes sense?
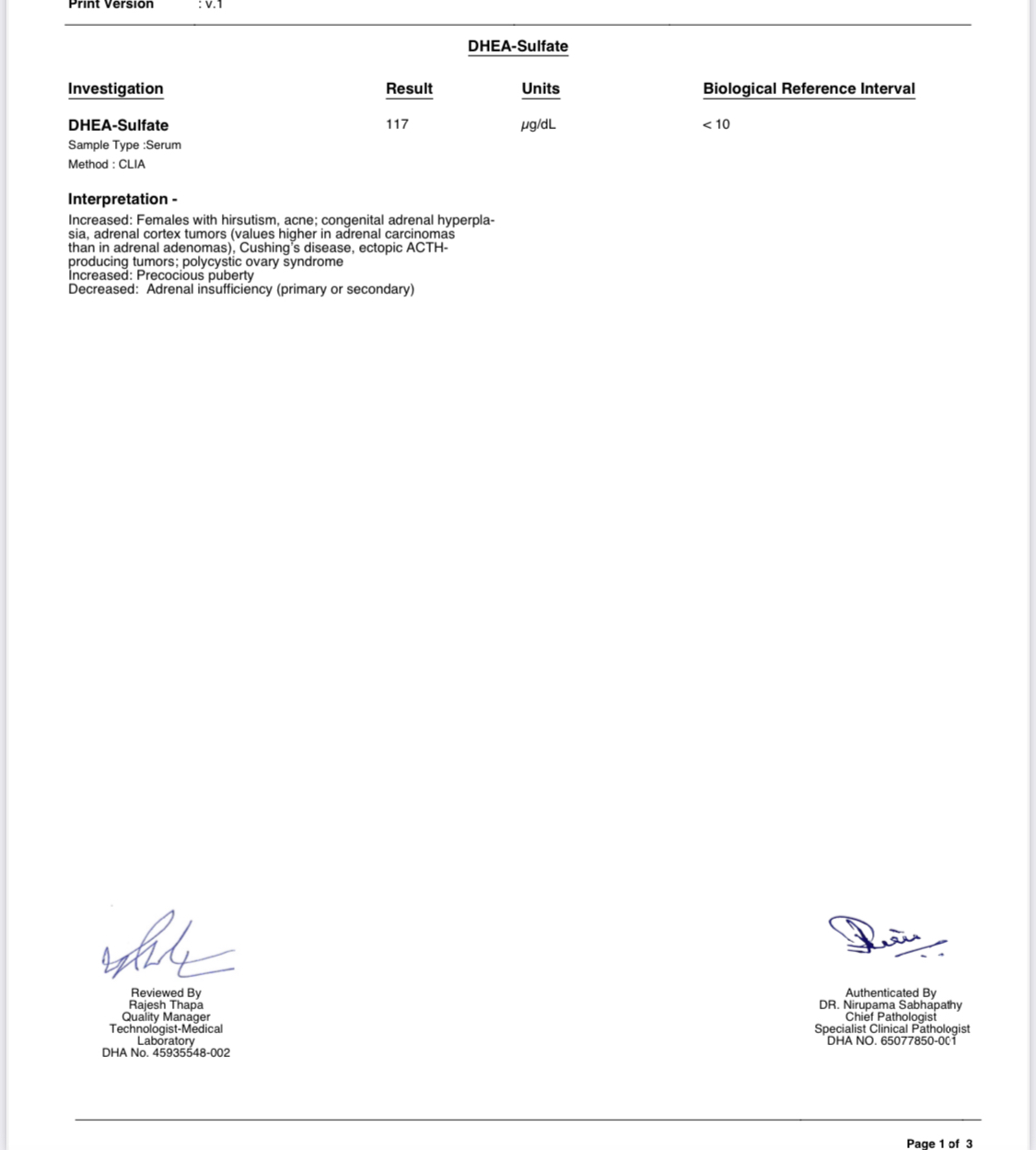
Now your test results show significantly elevated DHEAs. As you learned in the video I shared above, DHEA is a major androgen for women to produce testosterone. And elevated DHEA is one of the main contributing factors for acne (also mentioned in the handout above).
Therefore, the next question to be asking is ‘why is your body producing high levels of DHEA’?
Since you now know it’s made in the adrenal glands and its role is to protect us from the effects of cortisol, the first question I have to ask you is about stress.
What is your perceived level of stress?
High insulin (from stress and/or diet) can also increase DHEA. Have you tested your blood sugar levels including fasting insulin? (i.e. fasting glucose, HbA1C, fasting insulin)
Certain medications can increase DHEA. So can alcohol. Are you consuming any of these?
An overactive thyroid can also increase DHEA. Do you have any other symptoms that could point to hyperthyroid function? Watch THIS video from the Thyroid Balance course. Has a full thyroid panel been tested? Here are the markers.
PCOS. Has a gynecologist ever diagnosed you with PCOS?
Higher than normal body fat/obesity. Fat is an endocrine tissue, which can reduce sex hormone binding globulin (SHGB). SHGB has an affinity for binding to androgen hormones like DHEA and testosterone so if it’s low, there will be more DHEA circulating around having effect.
Another interesting clue that you shared is about acne coming out mid-cycle around ovulation. When we ovulate (assuming we release an egg), we produce A TON of progesterone in the second half of our cycle, called the luteal phase. Progesterone should naturally be higher than estrogen in the 2nd half of our cycle.
If however we do not ovulate, progesterone does not get produced, and we will be more estrogen dominant (higher ratio of estrogen to progesterone, even if levels look “normal” on labs).
So it is possible for a woman to be both androgen and estrogen dominant in different phases of her cycle, which is often the case in PCOS. (read more about it HERE in the Symptom Dictionary handout).
The above will help you figure out hormonal imbalances. But there are also other factors which may also be contributing to acne which we can explore as well, especially since you’ve been struggling with acne almost lifelong.
Have you ever measured your zinc levels? I would request RBC zinc and RBC copper together since they compete with each other.
Do you consume a lot of iron? Supplement with iron? Cook in cast iron? Iron opposes zinc.
Have you measured your vitamin A levels?
Have you measured RBC magnesium level?
Have you explored food sensitivities (especially dairy and gluten)? Have you ever done an elimination challenge to remove the most common culprits before? If you’re interested in testing, I would recommend the KBMO but it’s expensive!
Toxicity affecting detox pathways (i.e. mold & mycotoxins, agrichemicals, heavy metals). If you suspect this could be at play, I’ll share further action steps. Let me know.
Dysbiosis (imbalance in gut microbiome). Do you have any other GI symptoms that could point to that possibility like gas, bloating, reflux, heartburn, constipation, diarrhea?
Ok, I’ll leave it here for now. Please take the time to review the handouts/videos I’ve shared, and I’ll wait for your responses which you can reply to 1 by 1 since I’ve numbered them to help keep track. Awaiting your responses.
-
@Bernadette Abraham thank you so much for all this . I will tackle one by one and ask some additional questions and give you more info if needed
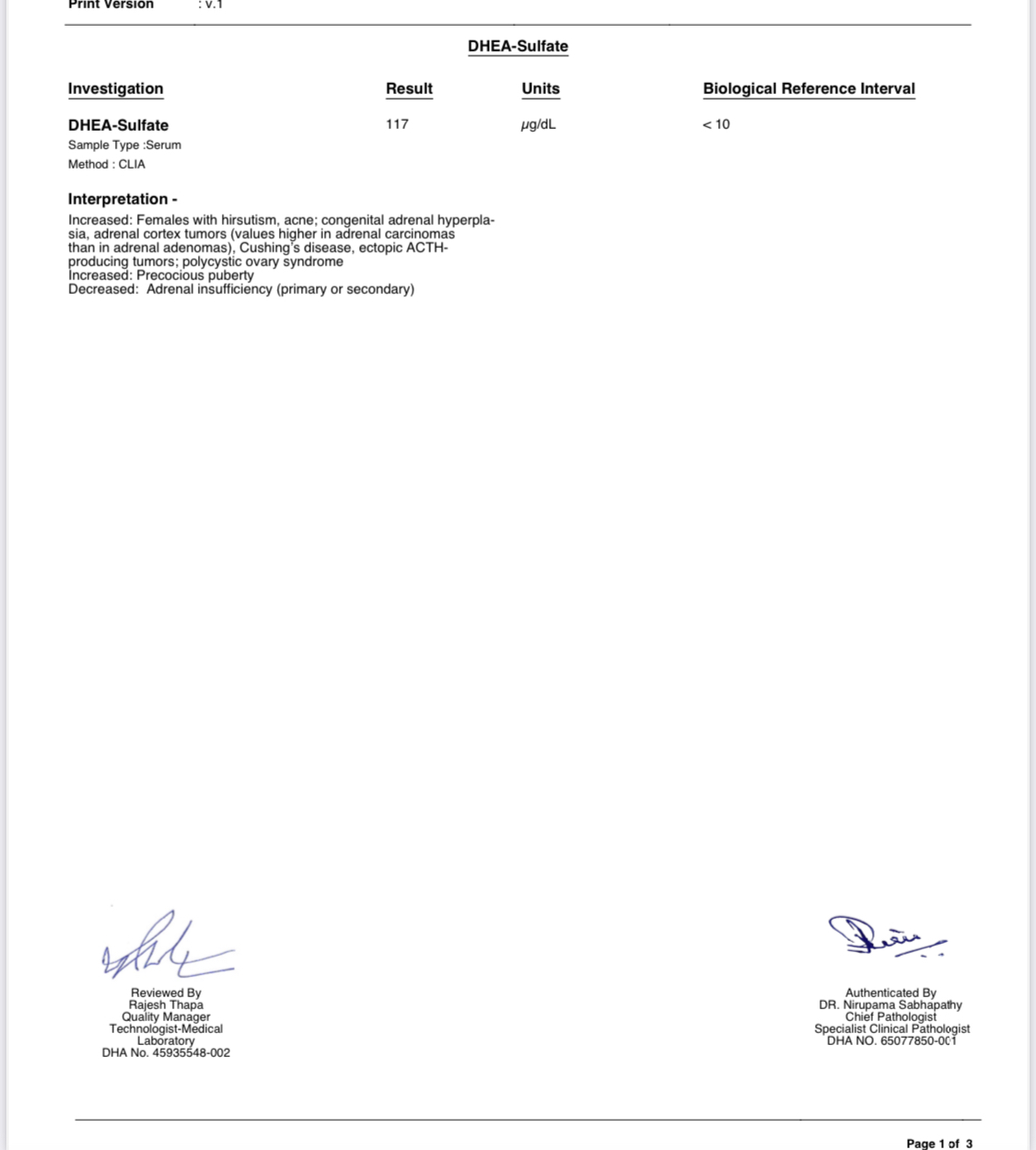
First of all I just received further horomone testing which I will attach at the bottom of my replies here . Just a small note : 2 months ago my progesterone was super low (.58 only ) and I was put on an adrenal protocol . So am glad to see it go up now. My DHEA-S was 97, now it went up to 107. Interetsing you say that my DHEA -S is so high , I was under the impression that it’s actually low !
I want to ask 2 things before I reply to yours
do you reccomend that I dog deeper and get a Dutch test done ? It’s pretty pricey so I want to know if it will help me further or are things clear from the blood tests I did ?
Is being androgen dominant heriditay ? And if so what I can do to reverse it in my daughter ?
Your replied below
Stress level : it’s ok . I have a stressful life and job and I have had quite a difficult year . I think my progesterone went down due to this . The last 2 months I am feeling much better with the adrenal program I was on
I don’t have insulin resistance no , I get tested
I don’t drink much , maybe once a week if I do and like one or 2 glasses of wine
Thyroid :.L actually my thyroid was under active , but we test it regularly /‘d it’s been stable
I have been diagnosed with PCOS yes . Also I should add that ever since I was a teenager I suffer from excess facial hair
I suffer from being underweight rather than overweight .
I never got tested for zinc no , I can certainly do it if you think it wouod help
I don’t cook in cast iron and I don’t take iron although in the past I did
Never tested vita A no . Though when I read some comments here I started looking into it via Valeo. Some research online says the serum is useless cos most vita a is stored in liver ? Again am fed it and desperate so if this help I wouod do it !
Never got tested for RBC magnesium
11. I don’t have gut issues and I don’t have food intolerance as far as I know . When I get flare up I try to cut dairy which is usually only kefir cottage cheese and butter
12. I had mold recently and was put for a protocol and has heavy metals and also went through chelation a few years ago and had a horrible acne reaction so I stopped half way . I really do think that my issue with acne is with androgens cos it’s around a ovulation and it stopped completely when I got pregnant and hence was not ovulating
-
@Yasmin atassi
Regarding lab value results. Please keep in mind that each lab has its own reference ranges and they can vary wildly from one lab to another. Based on what you shared above, the reference range for DHEAs showed <10 (which in itself seems odd/low because typical DHEAs for adult females is between 35-430 µg/dL). If < 10 is the reference range, then yes, a value of 117 ug/dL is considered highly elevated. But like I said, that RR does seem a bit odd. Please check previous lab test results from the same lab (check the units and reference range) and let me know if it’s the same or different. I wouldn’t warrant a DUTCH test at this stage, because there seems to be a lot more foundational issues needing to be addressed first that are directly impacting hormones. And no androgen dominance is not “genetic” per se. But there might be hereditary components that can influence hormone production, regulation, and sensitivity, which might predispose a person to conditions associated with androgen dominance, such as polycystic ovary syndrome (PCOS). It’s hormonal imbalance that can be caused by so many factors that “may” have genetic factors at play. Makes sense? Stress is a key factor. I’m glad you’re starting to feel better, but really continue to focus your efforts on mitigating stress as much as possible. Delegate, say no more often, ground daily, sleep early, journal/deep breathing, meditate, etc. Would you mind sharing your results for fasting glucose, fasting insulin and HbA1C? Given the PCOS diagnosis, insulin is very often a big factor. Just want to make sure it’s not being overlooked (it often is in the conventional world). Would you be willing to give up alcohol completely for at least 4 months to give your liver, immune system & hormones/neurotransmitters a break? Think of it as a stress on the body, which as I mentioned in #1, needs to be prioritized. There are stressors we cannot control in life, but I encourage controlling the ones that we can control. Alcohol is one of those stressors. Regarding thyroid function. It’s not uncommon for the thyroid to swing between hyper and hypothyroid function, especially if the adrenals are taxed (again from stress). During ovulation, if progesterone is not produced, we can become estrogen dominant, and transiently hypothyroid since estrogen increases TBG (thyroid binding globulin) which binds to thryoid hormone and can make a person feel hypothyroid transiently (meaning not all the time, but in phases of the cycle). PCOS increases androgen hormone production, hence the facial hair growth. As I mentioned in #4, stress (adrenal hyperfunction) can lead to thyroid hypofunction which is one of the root cause factors for PCOS. Please watch THIS VIDEO to better understand the different mechanisms how stress/cortisol affects hormone balance. Is your calorie consumption low? Do you overexercise? And refer to #4 regarding thyroid function. It’s also possible to have swings in both directions. 9. 10. Yes, worth getting RBC zinc, RBC copper (if available), RBC magnesium, and vitamin A tested. These are all critical for immune health, thyroid conversion and skin health. 11. Food intolerance and food sensitivities are different. An intolerance is generally felt in the gut. A sensitivity can show up days later and present itself all over the body. Please read THIS HANDOUT for possible symptoms. If you have any of these symptoms, consider an elimination challenge. Here’s the handout with more info on how to do that. I’d start with the most common culprits: gluten, dairy, corn, soy, yeast, citrus fruits, nuts, seeds, nightshades. These can be done all at once or individually by category. It’s up to you. If done all at once, search for “AIP” recipes online to help you put together a meal plan. I can help you further with this as well. Just let me know. If you weren’t able to tolerate the chelation therapy, you might want to try our upcoming Cleanse & Heavy Metal Detox Program. This also tells me that your elimination pathways need support. What cannot come out of the body, will come out through the skin. My assumption based on these threads is that you probably have a few root cause reasons at play, which I’ll briefly summarize below and then give you an action plan to consider: Stress > affecting thyroid function > increasing androgens > leading to annovulation > reduced progesterone > leading to estrogen dominance which can contribute to PCOS
PCOS (please report back on fasting insulin) > increases androgens
Toxicity > affecting elimination pathways > leading to acne
Possible food sensitivities (still undetermined but likely)
Possible nutrient insufficiencies (to be tested)
So where do you start?
a) Stress reduction!! Please read THIS HANDOUT on stress realities and reduction strategies.
b) Work on opening up your elimination pathways. Watch THIS VIDEO on opening up your drainage pathways. And then THIS VIDEO on which ones to prioritize first. You can also take THIS self-assessment to help you determine which pathways is weakest for you. And if you haven’t already, here are some markers to test liver/gallbladder function.
c) Do an elimination challenge (all at once or one category at a time).
d) get those additional tests to confirm/rule out if they are contributing to the problem
Hope this helps.
-
@Bernadette Abraham
Thank you . Regarding the lab results of DHEA-S I did it 2 months ago with the same lab ( via Valeo ) and I think the lab reverence’s are the same . I will check my files and let you know .
How do you find Valeo ? Are they reliable ? Am finding them the most cost effective with out of pocket tests but if you have any other suggestions pls let me know as I am in touch with them regarding the vitamin A , zinc and copper that you recommended ( by the way they don’t have Copper RBC)
I will send you my insulin tests . They are not made via conventional medicine , so I think they are fine
Hmm cutting alcohol completely is not pleasant lol ! I don’t generally have a lot but eveyone in a while I like to have it as a “mood” . But I will keep your advice in mind
I would say my calowire intake is low yes . I am trying my best to increase it bit honestly it’s hard work for me and it takes a lot of energy to focus on it
Thai was a helpful of handout cos some of those things ( sinus heavy head etc ) I def get from time to time and I always assumed it was from dusty weather i. Am a little worried of eliminating so many things and losing even more weight . Any help or strategy you can provide would be appreciated
just one thing : you mentioned anovulation : I do ovulate ( maybe last month I didn’t and hence my period was later and cos progesterone was low ) I have a pretty decent cycle length and my progestrone in the past was alsways ok never as low as 0.58 . I think that was truly ass a result of a very stressful last couple of months
-
@Bernadette Abraham here is the other dheas test I did 2 months with the lab references they out as different ( same lab ). I guess then the new one is an error from their side ..
-
@Yasmin atassi thanks for sharing the additional labs and info. I’ll reply one by one again.
Yes, it seems the RR for DHEA was off in your latest test in comparison to the other tests. I’d let Valeo Health know about that. I do like Valeo Health since they cut out the middle man and offer very reasonably priced tests. They also offer B Better members a discount, did you know? Here’s more info on that.
Life Pharmacy Clinics also have amazing packages for basic blood tests. Definitely give them a call for price comparison because I believe they’re even cheaper.
Thanks for sharing the fasting glucose and insulin results. Do you wake up full of energy or is it hard to get out bed? Do you follow a low-carb/keto diet? If you had no symptoms at all and were feeling great, I wouldn’t look into these values too much, however both your fasting glucose and fasting insulin are both suboptimally low. Since these are done in a fasting state and are dependent on the health of the adrenal glands and your CAR (cortisol awakening response), I’m suspicious of the possibility of adrenal hypofunction (slow functioning) impacting the release of glucose and therefore insulin. Would you be open to doing a 2-hour glucose tolerance test? This would provide better insights into blood sugar regulation. I know you mentioned that you felt better on an adrenal protocol. Are you still working on that?
If you’d like to test adrenal function, I share 3 ways to do so:
At home
In blood
In urine (DUTCH Plus would be my preferred test if budget allows)
If cutting alcohol for good sounds too daunting, consider removing it for 1 month to see how it makes you feel. You may be more motivated in doing so after noticing the difference in how it makes you feel after removal and reintroduction.
What exactly is the issue with the low-calorie intake? Do you skip meals? Are your portions very small? Do you avoid certain food groups? Please share more details about your diet and I can help you further. I would suggest you start a new post just about your diet as this one is getting crowded.
So again, I suggest starting a new post to just focus on your diet. If the AIP diet is too daunting, then I suggest removing 1 food group at a time. So for example, remove dairy for at least 1 month (100% removal, not even 1 bite or mistake). Then reintroduce dairy the proper way. Here’s a handout that discusses reintroductions after an elimination. This will hopefully make it feel more manageable. But again – please start a new thread, and let’s help you a bit more with the diet piece.
I’m recopying the action steps from my previous thread and adding a bit to it to realign. Please let me know if you have any questions about that.
So where do you start?
a) Stress reduction!! Please read THIS HANDOUT on stress realities and reduction strategies. Given the suboptimal fasting glucose and insulin, it may be worth testing adrenal function for a more detailed look. Please email support@bbettermembership.com if you need access to order the DUTCH Plus.
b) Work on opening up your elimination pathways. Watch THIS VIDEO on opening up your drainage pathways. And then THIS VIDEO on which ones to prioritize first. You can also take THIS self-assessment to help you determine which pathways is weakest for you. And if you haven’t already, here are some markers to test liver/gallbladder function.
c) Do an elimination challenge (all at once or one category at a time). As suggested, please start a new post and we can focus on diet only.
d) get those additional tests to confirm/rule out if they are contributing to the problem. As mentioned, call Life Pharmacy Clinics for price comparison.
-
@Bernadette Abraham hello Bernadette as per your advice I got my blood tests back pls see here and let me know your advise
-
@Yasmin atassi Aha! Ok, we’re getting some root cause answers! Zinc is clinically low, and vitamin A is suboptimal low (you can see it’s near the lower end of the reference range instead of being in the upper 2/3rds of the range)! And both of these nutrients are critical for skin health and immune health.
So the next question is why would zinc be low? Are you vegan or consume little animal proteins? Do you smoke (cadmium can replace zinc in the body)? Please watch THIS video on other risk factors for low zinc from our Mineral Balance course. Let me know what you suspect might be at play in your case. Correcting a zinc deficiency (watch THIS video) will likely be helpful in many ways, but ultimately, we have to figure out why you’re not getting in enough zinc into cells.
The same goes for vitamin A. Is it diet related? It is liver/gallbladder related? Vitamin A is a fat-soluble vitamin so if you’re getting in enough in your diet, is it a fat absorption issue due to issues with bile production and/or flow? You can fill in this short assessment form to help determine if gallbladder issues might be at play, and if you should test liver function. Please let me know your score.
Liver is an excellent source of vitamin A. My favorite supplement source of vitamin A is cod liver oil by Rosita.
-
@Bernadette Abraham thanks B . I don’t smoke ; I quit 12 years ago . And I eat plenty of animal protein. Maybe I could use to bring it up a notch to make it the 30g but I general I make sure I eat anima protein at every meal
Am Wondering whether this was a a result of breastfeeding – I stopped in February after 14 months – but since I was exclusively pumping I produced a lot of milk , and was severely underweight – things are much better now but I just wonder if that’s what caused it ?
Honestly I can’t think of anything in my diet ..
Since 2 weeks I have been taking 2 capsules of this , what do your think ? ( bood test is as taken before I started (
For vitamin A I try to take beef liver every now and then. But I did have issues with low bile in the past so maybe that can be the cause. I took the test and it was 0 for all answers .
I look forward to hearing from you
-
Also @Bernadette Abraham i am traveling soon and don’t have time order the vitamin a you suggested – I have the seeking health vitamin a liquid one in my cabinet . Wouod it be ok to start taking this and what space you reccomend and for how long ?
-
@Yasmin atassi yes, breastfeeding can definitely deplete your stores of zinc. So definitely make an effort to replenish those levels and retest your zinc levels in ~3 months if you choose to do so with supplementation. Typically, I’ll have my clients take 30-45mg zinc only for 30 to 60 days depending on how severe their deficiency is, and then switch to a zinc/copper blend (ex. Jarrow Zinc Balance) for another 1-2 months or so as needed.
As for the Rosita cod liver oil, it’s actually available in Dubai at that link I shared above so hopefully you can get it before travelling. But the one by Seeking Health is also a good brand. As for the duration, again, re-test in ~2-3 months to help you determine sufficiency.
-
@Bernadette Abraham Thanks so much / one last question : what would be the daily vitamin A dosage you recommend for my case ?
-
@Yasmin atassi I cannot provide specific dosage recommendations as I do not know your full health history. However I can provide general guidelines.
For non-pregnant women, the general recommendation to help raise suboptimal low levels is ~5000-7000 IU per day for 1-3 months. This would equate to ~2 tsp of the cod liver oil (liquid). And then retest in 2 months to see how levels are progressing and if there’s a need to stop or continue.
Hope that helps give you better direction.
Log in to reply.